Abstract
Background
With the increasing accessibility of next-generation sequencing (NGS), many institutions are incorporating routine mutational profiling to assist in the evaluation of patients with a variety of hematologic disorders, including cytopenias. Such testing can be helpful in distinguishing neoplastic causes of cytopenias from others. Mutation profiling of peripheral blood is a particularly attractive option because of its potential application as a minimally invasive screen for hematologic malignancies, particularly myeloid neoplasms. However, it is not entirely clear how such molecular data can inform hematology practice as there is limited data on the clinical value of routine NGS testing in cytopenic patients. Here we report the clinical utility of peripheral blood screening by targeted NGS testing in a large institutional cohort of patients with cytopenias.
Methods
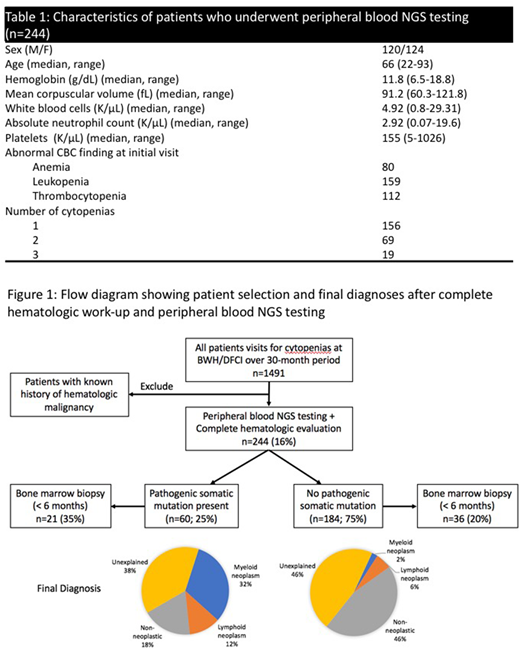
After institutional review board approval, we identified all patients presenting with peripheral blood cytopenias over a 30-month period (January 2015 - June 2017) to the Adult Hematology Clinic at Dana-Farber/Brigham and Women's Cancer Center (n=1491). Of these, 244 patients (median age: 66, range: 22-93) underwent testing of a peripheral blood specimen using a custom 95-gene, amplicon-based sequencing panel (Rapid Heme Panel, Kluk et al., 2016) surveying genes recurrently mutated in hematologic malignancies (Table 1). In addition, these patients also received a complete hematologic work-up to determine the cause for the cytopenia(s). All patients with a known history of a hematologic malignancy were excluded.
Results
Overall, 60 (25%) patients had a pathogenic somatic mutation in at least one of the 95 genes studied (Figure 1). An underlying hematologic malignancy was identified in 26 (44%) of these patients at the time of presentation, most commonly a myeloid neoplasm (19/26; 73%); 11 (18%) had a non-neoplastic etiology of the cytopenia(s); and 23 (38%) had unexplained cytopenia(s) following complete work-up. The most frequently mutated genes in patients with unexplained cytopenias were TET2, SF3B1 and SRSF2. Of the 184 (75%) patients without a pathogenic somatic mutation, 15 (8%) of these patients were found to have an underlying hematologic malignancy at the time of presentation, most commonly a lymphoid neoplasm (11/15; 73%); 84 (46%) had a non-neoplastic etiology of the cytopenia(s); and 85 (46%) had unexplained cytopenia(s) following complete work-up. With a median follow-up of 22 months, two patients with non-clonal unexplained cytopenias went on to develop MDS and splenic marginal zone lymphoma, respectively. Overall, the presence of a pathogenic mutation was strongly associated with the diagnosis of a myeloid neoplasm (RR 11.6, 95% CI 4.5-29.8). Conversely, if no pathogenic mutation were identified, the likelihood of developing a myeloid neoplasm in 2 years was low (5/184; 2.7%).
To further investigate the diagnostic utility of peripheral blood mutational profiling as a screening test in predicting the presence of a myeloid neoplasm on bone marrow biopsy, we studied its diagnostic characteristics using bone marrow biopsy diagnosis within a 6-month interval as the gold standard (n=57). The absence of a pathogenic mutation in peripheral blood was highly predictive of absence of a myeloid neoplasm on bone marrow biopsy (NPV 94%, 95% CI 84-99%). The presence of specific mutations in spliceosome genes (SF3B1, SRSF2, U2AF1) and co-mutation patterns involving DNMT3A, TET2 and ASXL1 genes and other genes were predictive of a myeloid neoplasm with positive predictive values of 75% (95% CI 41-93%) and 70% (95% CI 41-88%) respectively. Finally, larger clone sizes (≥20%) and higher numbers of mutations (≥2) were also predictive of a myeloid neoplasm (PPV: 80%, 95% CI 60-90% and 75%, 95% CI 49-90%, respectively).
Conclusions
In conclusion, mutation profiling of peripheral blood is a valuable minimally invasive test in the diagnostic work-up of the cytopenic patient. After a complete hematologic work-up and in the absence of a pathogenic somatic mutation, the likelihood of developing a myeloid neoplasm in 2 years is very low. Also, the lack of a pathogenic mutation in peripheral blood is highly predictive of the absence of a myeloid neoplasm on a bone marrow biopsy. Finally, certain molecular features (number and type of mutations, clone size) are predictive of a myeloid neoplasm.
Kim:LabCorp, Inc.: Consultancy; Papgene, Inc: Consultancy; Aushon Biosciences: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal